With that piece of information it seems far more likely that the liver is in play here. Good on you for stopping when you did.
Massive disclaimer: the following is extrapolation based on known relationships between exercise and liver disease on oxidative stress. As far as I can tell, there isn’t much in the way of studies for your particular case. Alcohol-induced impairment of aldehyde metabolism does not seem well-studied; lots of papers on alcohol-related liver disease, but the number of people with ALD who are attempting more than recreational exercise is going to be very small… not seeing any studies on this.
Regardless, I do suspect that your alcohol intolerance and your post-workout “hangovers” are related. Alcohol intolerance is largely an issue with not being able to deal with oxidative stress. And if there is a particular factor of exercise that increases with duration, intensity, and heat… it’s oxidative stress.
Two hypothetical pathways here involving impaired ability to deal with oxidative stress:
- Dysfunctional aldehyde metabolism via some kind of epigenetic factors. Heavy drinking can lead to acquired dysfunction of this pathway, but it may not be related to dysfunction of the enzyme itself.
- Impaired liver function due to alcohol-related liver damage (fibrosis/cirrhosis, mitochondrial damage, chronic inflammation). The liver is the major producer and central regulator of antioxidants. Your aldehyde metabolism could be working properly, but you could have less metabolic reserve to maintain overall redox balance. You’re good during most shorter exercises, but once the ROS generation reaches a certain point (via length, intensity, heat), your liver can’t keep up. This etiology implicates far more than aldehyde metabolism, but also the glutathione system, and a myriad of antioxidant enzymes.
Or both. #2 is going to be way more likely, stats-wise. I’d talk with your PCP about your history and see if you can get your labs drawn up for signs of alcohol-related liver disease and that whole differential (did alcohol cause the damage or was it something else that nuked your ability to tolerate the alcohol?). That would be the priority. The ethanol skin patch doesn’t mean much if negative, would be super interesting if positive.
Something you could try is supplementation of antioxidants to see if your symptoms improve. There’s mixed evidence antioxidant supplementation can help with a variety of liver diseases. That said, the end results measured were like all cause mortality, fibrosis, etc, not adverse reactions to exercise. I don’t see a major downside. Vitamin E, Vitamin C, and NAC are common interventions in these studies. All have a good safety profiles but of course [talk to your doctor if you have any contraindications disclaimer]. If you notice improvement, your symptoms might be ROS-related. If you don’t notice anything, not much can be read from that.
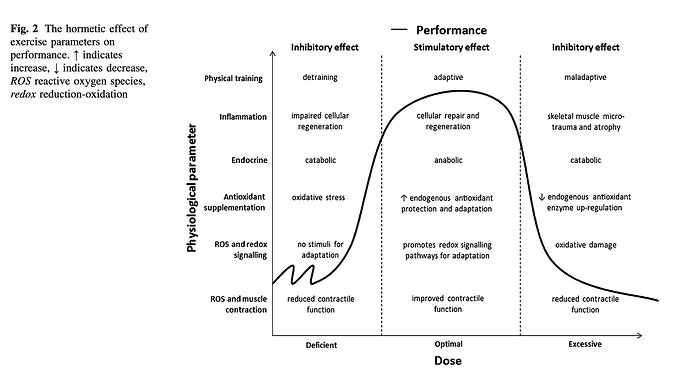
And before a bunch of other cyclists start thinking “oh, should I be supplementing a bunch of antioxidants too?” Probably not? You actually DO want some amount of oxidative stress from exercise for a hormetic response (a lot of poison is bad, but a little poison can be adaptive). There’s a decent amount of debate over whether antioxidant supplementation hinders athletic training stimulus. However in @DingoDongo’s case, some kind of impaired of antioxidant response could be pushing rigorous exercise into the “lotta poison bad” category.
As a final note, exercise has generally been found to be a positive intervention for improving ALD outcomes… however the amount of exercise studied is going to be more “we got sedentary people to do an 30-60mins of light cardio” not “3+ hours bike rides in the sweltering heat.”